How to Create a Healthy Eating Plan for Type 2 Diabetes
Type 2 diabetes is a chronic condition that affects millions of people worldwide. It is characterized by high blood sugar levels resulting from insulin resistance or inadequate insulin production. While medication and lifestyle changes are key to managing type 2 diabetes, a healthy eating plan plays a crucial role in controlling blood sugar levels and preventing complications.
In this comprehensive article, we will delve into the importance of creating a healthy eating plan specifically tailored for type 2 diabetes. We will explore dietary guidelines, nutritional needs assessment, meal planning strategies, and practical tips for making smart food choices.
By the end of this article, you will have the knowledge and tools to create a personalized and sustainable eating plan to effectively manage your type 2 diabetes. Let’s embark on this journey toward better health and improved diabetes management.
Understanding Dietary Guidelines for Managing Type 2 Diabetes
Diet plays a crucial role in managing type 2 diabetes. A healthy eating plan can help control blood sugar levels, manage weight, improve insulin sensitivity, and reduce the risk of complications. To achieve these goals, it is essential to adhere to dietary guidelines specifically designed for individuals with type 2 diabetes. Let’s explore these guidelines in more detail:-
1.Carbohydrates:
- Focus on complex carbohydrates: Choose whole grains, legumes, fruits, and vegetables that provide fiber and essential nutrients.
- Limit refined carbohydrates: Minimize or avoid foods made with white flour, sugar, and highly processed grains, as they can cause rapid spikes in blood sugar levels.
2.Protein:
- Include lean protein sources: Opt for lean meats, poultry, fish, eggs, and plant-based protein sources like tofu, legumes, and nuts.
- Control portion sizes: Aim for moderate amounts of protein with each meal to prevent excessive calorie intake.
3.Fats:
- Choose healthy fats: Opt for unsaturated fats found in foods like avocados, nuts, seeds, olive oil, and fatty fish.
- Limit saturated and trans fats: Reduce intake of fried foods, high-fat dairy products, fatty cuts of meat, and processed snacks that are high in unhealthy fats.
4.Portion Control:
- Be mindful of portion sizes: Use measuring cups, food scales, or visual cues to ensure appropriate portions of carbohydrates, proteins, and fats.
- Avoid oversized servings: Watch out for super-sized meals at restaurants and be cautious when consuming processed and packaged foods.
5.Meal Timing:
- Establish a regular eating schedule: Aim for consistent meal times to help regulate blood sugar levels and avoid long periods of fasting.
- Consider spacing out meals: Some individuals benefit from consuming smaller, more frequent meals, while others may prefer three balanced meals per day.
6.Hydration:
- Stay adequately hydrated: Drink plenty of water throughout the day to support overall health and assist in managing blood sugar levels.
It is important to note that individualized nutrition plans may vary based on factors such as age, gender, activity level, and existing health conditions. Consulting with a healthcare professional or registered dietitian can provide personalized guidance and support in developing a tailored eating plan that suits your specific needs.
Understanding the Impact of Diet on Diabetes Management
Diet plays a crucial role in managing type 2 diabetes. The food choices we make can have a direct impact on blood sugar levels, insulin sensitivity, weight management, and overall well-being.
1.Blood Sugar Control:
- Carbohydrate Management: Carbohydrates have the most significant impact on blood sugar levels. By choosing complex carbohydrates that are high in fiber and have a lower glycemic index, such as whole grains, legumes, and non-starchy vegetables, you can promote more stable blood sugar levels.
- Portion Control: Controlling portion sizes helps regulate the amount of carbohydrates consumed and prevents excessive spikes in blood sugar levels.
- Balanced Meals: Creating balanced meals that include a combination of carbohydrates, proteins, and healthy fats can help slow down the digestion and absorption of carbohydrates, leading to more stable blood sugar levels throughout the day.
2.Weight Management:
- Caloric Balance: Achieving and maintaining a healthy weight is important for managing type 2 diabetes. By following a balanced and calorie-controlled eating plan, you can manage your weight effectively.
- Nutrient-Dense Foods: Opting for nutrient-dense foods that are lower in calories and higher in essential nutrients can support weight management while providing optimal nutrition.
3.Insulin Sensitivity:
- Healthy Fats: Including healthy fats in your diet, such as monounsaturated and polyunsaturated fats found in foods like avocados, nuts, seeds, and olive oil, can improve insulin sensitivity.
- Protein: Consuming adequate amounts of lean protein sources helps promote satiety, support muscle mass, and improve insulin sensitivity.
4.Cardiovascular Health:
- Heart-Healthy Choices: A well-balanced eating plan that emphasizes whole grains, fruits, vegetables, lean proteins, and healthy fats can reduce the risk of heart disease, which is commonly associated with type 2 diabetes.
- Limiting Sodium and Saturated Fats: Reducing the intake of sodium and saturated fats from sources like processed foods, high-fat dairy, and fatty meats can help manage blood pressure and cholesterol levels.
5.Overall Well-being:
- Micronutrient Intake: Consuming a variety of nutrient-rich foods provides essential vitamins, minerals, and antioxidants that support overall health and well-being.
- Hydration: Staying adequately hydrated supports proper digestion, metabolism, and overall bodily functions.
It’s important to note that while diet is a critical component of diabetes management, it is not the only factor. Regular physical activity, stress management, and medication adherence also play significant roles. Consulting with a healthcare professional or registered dietitian is recommended to develop a personalized eating plan that suits your individual needs and goals.
Importance of Portion Control and Meal Timing in Type 2 Diabetes Management
Portion control and meal timing are two crucial aspects of managing type 2 diabetes effectively. They play a significant role in regulating blood sugar levels, promoting weight management, and optimizing overall health.
1.Portion Control:
- Blood Sugar Management: Controlling portion sizes helps regulate the amount of carbohydrates consumed at each meal. By managing carbohydrate intake, you can prevent excessive spikes in blood sugar levels and maintain more stable glucose control throughout the day.
- Caloric Balance: Portion control is also essential for weight management. By monitoring the total calories consumed, you can create an energy balance that supports achieving and maintaining a healthy weight. This is crucial because excess body weight can worsen insulin resistance and blood sugar control.
- Balanced Nutrition: Controlling portion sizes allows for a well-rounded meal that includes appropriate amounts of carbohydrates, protein, and healthy fats. This balance supports overall nutrition, satiety, and optimal energy levels.
2.Meal Timing:
- Blood Sugar Regulation: Establishing regular meal times and avoiding prolonged periods of fasting is beneficial for blood sugar regulation. Consistency in meal timing helps maintain stable blood sugar levels, preventing drastic fluctuations that can impact energy levels and overall well-being.
- Optimal Medication Effectiveness: Meal timing is particularly important for individuals who take medication, such as insulin or oral glucose-lowering drugs. By aligning meals with medication dosing, you can enhance the effectiveness of the medication and prevent hypoglycemia (low blood sugar) or hyperglycemia (high blood sugar) episodes.
- Sustained Energy Levels: Eating at regular intervals ensures a constant supply of nutrients and energy throughout the day. This can help prevent extreme hunger, overeating, and unhealthy food choices due to excessive hunger.
By incorporating portion control and meal timing into your daily routine, you can effectively manage blood sugar levels, support weight management goals, and improve overall diabetes control. Here are some practical tips to help you implement these practices:-
- Use measuring cups, food scales, or visual cues to estimate portion sizes.
- Read food labels to understand serving sizes and adjust accordingly.
- Divide your plate into appropriate portions for carbohydrates, proteins, and vegetables.
- Eat mindfully, paying attention to hunger and satiety cues.
- Plan your meals and snacks ahead of time to ensure regular eating intervals.
- Consider spreading out your carbohydrate intake throughout the day, rather than consuming large amounts in one sitting.
- Work with a registered dietitian to develop personalized meal plans and strategies that suit your specific needs and preferences.
Assessing Your Nutritional Needs for Type 2 Diabetes Management
To create a personalized and effective healthy eating plan for managing type 2 diabetes, it’s crucial to assess your individual nutritional needs. Understanding your specific requirements helps you tailor your diet to optimize blood sugar control, support weight management, and promote overall well-being. Here are key steps to assess your nutritional needs:-
1.Consult with a Healthcare Professional:
- Begin by consulting with a healthcare professional, such as a doctor or registered dietitian, who specializes in diabetes management. They can provide valuable insights and guidance based on your medical history, current health status, medications, and any specific concerns or dietary restrictions. Evaluate personal factors such as age, gender, weight, height, and activity level. These factors influence your calorie needs and nutrient requirements. For instance, older adults may have different nutritional needs compared to younger individuals, and physical activity levels impact energy expenditure and nutrient needs.
2.Consider Personal Factors:
- Evaluate personal factors such as age, gender, weight, height, and activity level. These factors influence your calorie needs and nutrient requirements. For instance, older adults may have different nutritional needs compared to younger individuals, and physical activity levels impact energy expenditure and nutrient needs.
3.Assess Current Eating Habits:
- Take an honest look at your current eating habits. Keep a food diary for a few days to track what and how much you eat. This helps identify areas for improvement, such as excessive portions, frequent consumption of high-sugar or high-fat foods, or inadequate intake of certain nutrients.
4.Blood Sugar Monitoring:
- Regularly monitor your blood sugar levels to understand how different foods and eating patterns affect your glucose control. This can provide valuable feedback on what foods or portions may cause spikes or dips in blood sugar levels, allowing you to make necessary adjustments to your diet.
5.Nutrient Requirements:
- Determine your specific nutrient requirements. These include macronutrients (carbohydrates, protein, and fats) and micronutrients (vitamins and minerals). Aim to meet your individual needs for each nutrient, considering any specific recommendations provided by your healthcare professional.
6.Individualize Your Plan:
- Once you have assessed your nutritional needs, work with a registered dietitian who specializes in diabetes management. They can help develop a personalized eating plan that considers your specific needs, preferences, and lifestyle. This plan will incorporate appropriate portion sizes, macronutrient distribution, and food choices to optimize blood sugar control and overall health.
7.Regular Follow-Up:
- Regularly follow up with your healthcare professional or dietitian to monitor progress, address any concerns or challenges, and make necessary adjustments to your eating plan. Diabetes management is an ongoing process, and personalized guidance can help ensure long-term success.
Assessing your nutritional needs and working with healthcare professionals, you can create a tailored eating plan that supports your individual goals for managing type 2 diabetes. Remember, everyone’s nutritional needs may vary, so it’s important to seek personalized advice and regularly review and adapt your eating plan as needed.
Consulting with a Healthcare Professional or Dietitian
Consulting with a healthcare professional or dietitian is a crucial step in managing type 2 diabetes and creating a healthy eating plan. These experts have the knowledge and expertise to provide personalized guidance based on your specific needs, medical history, and goals. Here are some key reasons why consulting with a healthcare professional or dietitian is important:-
1.Personalized Guidance:
- Healthcare professionals and dietitians can assess your unique health situation and provide tailored recommendations. They take into account factors such as your current health status, medications, blood sugar control, dietary preferences, and lifestyle to develop a customized eating plan that suits you.
2.Expert Knowledge:
- Healthcare professionals and dietitians specialize in diabetes management and nutrition. They stay updated on the latest research and guidelines, ensuring that the advice and recommendations they provide are based on evidence-based practices. This expertise helps ensure the accuracy and effectiveness of the guidance you receive.
Blood Sugar Monitoring and Medication
3.Management:
- Healthcare professionals can guide you on how to monitor your blood sugar levels effectively. They can help interpret the results, identify patterns, and make appropriate adjustments to your eating plan or medication regimen as needed. This helps optimize blood sugar control and prevent complications.
Addressing Individual
4.Challenges:
- Each person faces unique challenges when managing type 2 diabetes. Whether it’s managing weight, understanding food labels, overcoming emotional eating, or navigating social situations, healthcare professionals and dietitians can provide strategies and support to help you overcome these challenges.
5.Long-Term Support and Accountability:
- Regular follow-up appointments with healthcare professionals or dietitians provide ongoing support and accountability. They can track your progress, answer your questions, provide education, and make necessary adjustments to your eating plan as your needs evolve over time. This support is invaluable in maintaining long-term success in diabetes management.
Remember, healthcare professionals and dietitians are part of your healthcare team. They work collaboratively with you to develop a comprehensive approach to managing type 2 diabetes, which may include diet, exercise, medication, and other lifestyle modifications. Their expertise and guidance complement your efforts and increase the likelihood of achieving your health goals.
Benefits of Personalized Guidance
- Optimized Blood Sugar Control.
- Nutritional Adequacy.
- Practical Strategies.
- Holistic Approach.
- Helps you stay motivated, track your progress, address any concerns.
- Make you informed decisions about your diet and navigate potential complications.
- Provides strategies and support tailored to your specific challenges.
- Provides specific recommendations on carbohydrate intake, allowing for better blood sugar control and meal planning.
- Provides strategies for achieving and maintaining a healthy weight.
Setting Realistic Goals for Blood Sugar Control in Type 2 Diabetes

When managing type 2 diabetes, setting realistic goals for blood sugar control is essential. These goals provide a target for you to work towards and can help guide your diabetes management plan. Here are some key considerations for setting realistic goals:-
1.Consult with Healthcare Professionals: Work closely with your healthcare team, including your doctor and/or diabetes educator, to determine appropriate blood sugar targets based on your individual circumstances. They can provide guidance based on factors such as your age, overall health, duration of diabetes, and any existing complications.
2.Understand Blood Sugar Targets: Learn about the different blood sugar targets and what they mean. The common blood sugar targets for adults with type 2 diabetes are:
- Fasting Blood Sugar (before meals): 80-130 mg/dL (4.4-7.2 mmol/L)
- Postprandial Blood Sugar (after meals): <180 mg/dL (<10.0 mmol/L)
- Consider Personal Factors: Take into account your personal circumstances, such as your lifestyle, preferences, and daily routine. Set goals that are realistic and manageable for you. For example, if you have a busy schedule, consider how your blood sugar goals fit into your daily activities.
3.Gradual Progression: Start by setting small, achievable goals that can be gradually improved upon. Trying to achieve drastic changes in blood sugar control can be overwhelming and may not be sustainable in the long term. Celebrate small victories along the way to stay motivated.
4.Balance Blood Sugar Stability and Quality of Life: Strive for blood sugar stability while also considering your overall quality of life. It’s important to find a balance that allows you to manage your blood sugar effectively without feeling restricted or deprived. Work with your healthcare team to strike this balance.
5.Individualize Goals: Set goals that align with your unique needs and circumstances. For example, if you have other health conditions or limitations, your blood sugar goals may need to be adjusted accordingly. Personalize your goals to ensure they are achievable and relevant to your situation.
6.Track and Monitor Progress: Keep a record of your blood sugar readings and regularly review them with your healthcare team. This helps track your progress, identify patterns, and make any necessary adjustments to your diabetes management plan.
7.Celebrate Progress: Acknowledge and celebrate your achievements as you work towards your blood sugar goals. Recognize the efforts you put in and the positive changes you make to manage your diabetes effectively. This can help keep you motivated and committed to your long-term goals.
Understanding Macronutrients and Their Impact on Diabetes
Macronutrients, including carbohydrates, proteins, and fats, play a crucial role in the management of diabetes. Each macronutrient has a unique impact on blood sugar levels and overall health, making it important to understand their effects and incorporate them appropriately into a diabetes-friendly eating plan.
Carbohydrates, in particular, have the most significant impact on blood sugar levels. When consumed, carbohydrates are broken down into glucose, causing a rise in blood sugar. For individuals with diabetes, it is essential to monitor and manage carbohydrate intake to maintain stable blood sugar levels. Choosing the right types of carbohydrates, such as whole grains, legumes, and vegetables, can help promote better blood sugar control due to their slower digestion and lower glycemic index.
Proteins, on the other hand, have a minimal effect on blood sugar levels. They provide essential amino acids for cell repair and maintenance, support satiety, and help stabilize blood sugar levels by slowing down the digestion and absorption of carbohydrates. Including lean sources of protein such as poultry, fish, tofu, and legumes in meals can help balance blood sugar levels and support overall health.
Fats also play a role in diabetes management. While fats do not directly affect blood sugar levels, they can impact overall insulin sensitivity and cardiovascular health. It is important to choose healthy fats, such as those found in avocados, nuts, seeds, and olive oil, while limiting saturated and trans fats, which can contribute to insulin resistance and increase the risk of heart disease.
Balancing macronutrients is key in diabetes management. A personalized approach, considering factors such as individual blood sugar targets, medications, and activity levels, is crucial to determining the optimal distribution of macronutrients in an individual’s eating plan. Working with a healthcare professional or registered dietitian who specializes in diabetes management can provide personalized guidance on the appropriate amounts of carbohydrates, proteins, and fats to include in meals, considering individual needs and preferences.
In summary, understanding the impact of macronutrients on diabetes is vital for effective blood sugar control. By monitoring and balancing carbohydrate intake, incorporating adequate protein, and choosing healthy fats, individuals with diabetes can optimize blood sugar levels, support overall health, and achieve long-term diabetes management goals.
Carbohydrates and Their Effect on Blood Glucose Levels in Diabetes
Carbohydrates have a significant impact on blood glucose levels, making them a crucial consideration for individuals with diabetes. When consumed, carbohydrates are broken down into glucose, which is the primary source of energy for the body. This process causes blood sugar levels to rise. Understanding the different types of carbohydrates and their effects can help individuals with diabetes manage their blood glucose levels effectively.
1.Simple Carbohydrates:
Simple carbohydrates are made up of one or two sugar molecules and are quickly digested and absorbed by the body, leading to rapid spikes in blood glucose levels. Foods high in simple carbohydrates include sugary beverages, candy, desserts, and processed snacks. Consuming these foods can cause a sudden surge in blood sugar levels, which may be challenging to manage for individuals with diabetes.
2.Complex Carbohydrates:
Complex carbohydrates consist of longer chains of sugar molecules and take longer to digest and absorb. This slower digestion results in a more gradual release of glucose into the bloodstream, leading to a more stable and controlled rise in blood sugar levels. Examples of complex carbohydrates include whole grains, legumes, starchy vegetables, and fiber-rich foods.
3.Fiber:
Fiber is a type of carbohydrate that is not digested by the body. It passes through the digestive system largely intact, providing various health benefits, including better blood sugar control. High-fiber foods, such as fruits, vegetables, whole grains, and legumes, can help slow down the absorption of glucose, preventing rapid spikes in blood sugar levels and promoting overall glycemic control.
4.Glycemic Index:
The glycemic index (GI) is a scale that ranks carbohydrates based on their impact on blood sugar levels. Foods with a high GI value, such as white bread and sugary cereals, are rapidly digested and cause a quicker rise in blood sugar levels. On the other hand, foods with a low GI value, such as whole grains, legumes, and non-starchy vegetables, are digested more slowly, resulting in a gradual increase in blood glucose levels.
Managing carbohydrate intake is a key component of blood glucose control for individuals with diabetes. Consistency in carbohydrate consumption, portion control, and choosing healthier carbohydrate sources can help regulate blood sugar levels. It is important to work with a healthcare professional or registered dietitian who specializes in diabetes management to determine an appropriate carbohydrate intake that aligns with individual needs, preferences, and blood sugar targets.
Protein and Its Role in Managing Satiety and Blood Sugar Control
Protein plays a vital role in managing satiety and blood sugar control for individuals with diabetes. Including adequate protein in meals can have several beneficial effects on appetite regulation, glucose metabolism, and overall diabetes management.
Here are some key points regarding protein and its role in managing satiety and blood sugar control:-
1.Satiety and Appetite Regulation:
- Protein has a higher satiety value compared to carbohydrates and fats, meaning it helps you feel fuller for longer after a meal. By including protein-rich foods, such as lean meats, poultry, fish, eggs, dairy products, tofu, and legumes, in your meals, you can promote feelings of fullness and reduce the likelihood of overeating or snacking on unhealthy foods. This can be particularly helpful for weight management, as excess weight can impact insulin sensitivity and blood sugar control.
2.Glucose Control:
- Protein has a minimal effect on blood sugar levels compared to carbohydrates. When consumed, protein does not cause a significant increase in blood glucose levels or require large amounts of insulin for processing. This makes protein a valuable component of meals for individuals with diabetes, as it helps prevent sudden spikes in blood sugar levels. By balancing protein intake with carbohydrates, you can achieve a more gradual release of glucose into the bloodstream, promoting better glycemic control.
3.Glucagon Release:
- Protein consumption triggers the release of glucagon, a hormone that helps regulate blood sugar levels. Glucagon works in opposition to insulin, promoting the breakdown of glycogen (stored glucose) in the liver and stimulating the production of new glucose. This process helps maintain a stable supply of glucose in the bloodstream, preventing hypoglycemia (low blood sugar) and supporting overall blood sugar control.
4.Muscle Health and Insulin Sensitivity:
- Protein is essential for building and maintaining muscle mass. Regular consumption of adequate protein, combined with resistance exercise, can help preserve and enhance muscle strength and function. This is particularly important for individuals with diabetes, as muscle mass plays a significant role in insulin sensitivity. By maintaining optimal muscle health, you can improve insulin sensitivity, enhance glucose uptake by muscles, and improve overall blood sugar control.
5.Meal Composition and Timing:
- Including a source of protein in each meal and snack can help balance blood sugar levels and prevent rapid glucose spikes. Aim to distribute protein intake evenly throughout the day rather than consuming large amounts in one meal. Combining protein with carbohydrates and healthy fats in meals can further slow down digestion, promoting a more controlled release of glucose into the bloodstream.
In summary, including adequate protein in meals can help manage satiety, promote stable blood sugar control, and support overall diabetes management. By incorporating lean protein sources and balancing protein intake with carbohydrates, individuals with diabetes can optimize their dietary choices to achieve better appetite control and glycemic regulation.
Healthy Fats and Their Benefits for Heart Health
Contrary to popular belief, not all fats are bad for your health. In fact, incorporating healthy fats into your diet can have numerous benefits, particularly for heart health. Healthy fats provide essential nutrients and play a crucial role in maintaining optimal cardiovascular function.
Here are some key points highlighting the benefits of healthy fats for heart health:-
1.Source of Essential Fatty Acids:
Healthy fats, such as monounsaturated fats and polyunsaturated fats, are rich sources of essential fatty acids, including omega-3 and omega-6 fatty acids. These fats cannot be synthesized by the body and must be obtained through the diet. Omega-3 fatty acids, found in fatty fish (such as salmon and sardines), flaxseeds, chia seeds, and walnuts, have been extensively studied for their heart-protective benefits. They help reduce inflammation, lower triglyceride levels, and improve overall cardiovascular health.
2.Cholesterol Management:
Including healthy fats in your diet can help manage cholesterol levels. Monounsaturated and polyunsaturated fats have been shown to raise levels of high-density lipoprotein (HDL) cholesterol, often referred to as “good” cholesterol. HDL cholesterol helps remove low-density lipoprotein (LDL) cholesterol, or “bad” cholesterol, from the bloodstream, reducing the risk of plaque buildup in the arteries and the development of heart disease.
3.Reduced Risk of Heart Disease:
Consuming healthy fats as part of a balanced diet has been associated with a reduced risk of heart disease. Research has shown that replacing saturated and trans fats with monounsaturated and polyunsaturated fats can help lower the risk of heart disease and related complications. Healthy fats promote healthier lipid profiles, improved blood vessel function, and reduced inflammation, all of which contribute to better heart health.
4.Anti-Inflammatory Properties:
Chronic inflammation is a key contributor to the development and progression of cardiovascular disease. Healthy fats, particularly omega-3 fatty acids, possess anti-inflammatory properties that can help reduce inflammation in the body. By incorporating foods rich in healthy fats, such as avocados, olive oil, nuts, and seeds, you can help mitigate inflammation and support heart health.
5.Nutrient Absorption:
Certain vitamins, such as vitamins A, D, E, and K, are fat-soluble, meaning they require dietary fats for proper absorption. Including healthy fats in your meals can enhance the absorption of these essential vitamins, promoting overall health and supporting various bodily functions, including cardiovascular health.
6.Satiety and Weight Management:
Healthy fats provide a feeling of satiety and can help control appetite. Including moderate amounts of healthy fats in meals can contribute to better portion control and reduce the likelihood of overeating. This can be beneficial for weight management, as excess weight is a risk factor for heart disease.
In summary, incorporating healthy fats into your diet can provide significant benefits for heart health. By choosing the right sources of fats and practicing moderation, you can support cardiovascular well-being, manage cholesterol levels, reduce inflammation.
Designing Your Healthy Eating Plan for Type 2 Diabetes
Designing a healthy eating plan that suits your needs and helps manage type 2 diabetes is essential for maintaining optimal health and blood sugar control. Here are key considerations to keep in mind when creating your personalized eating plan:-
1.Balance and Variety:
Focus on incorporating a variety of nutrient-dense foods from different food groups. This includes whole grains, lean proteins, healthy fats, fruits, vegetables, and low-fat dairy products. Aim to have a balance of carbohydrates, proteins, and fats in each meal to promote stable blood sugar levels and provide a wide range of essential nutrients.
2.Carbohydrate Control:
Managing carbohydrate intake is crucial for individuals with type 2 diabetes. Consider the total amount of carbohydrates consumed in each meal and distribute them evenly throughout the day. Choose complex carbohydrates with a lower glycemic index, such as whole grains, legumes, and non-starchy vegetables, to prevent rapid spikes in blood sugar levels.
3.Portion Control:
Controlling portion sizes is key to managing calorie intake and blood sugar levels. Be mindful of serving sizes and use measuring tools to ensure accuracy. Pay attention to the total amount of food consumed, as even healthy foods can contribute to weight gain if portions are too large.
4.Healthy Fats:
Incorporate healthy fats into your eating plan, such as avocados, nuts, seeds, olive oil, and fatty fish. These fats provide essential nutrients and support heart health. However, remember that fats are calorie-dense, so moderation is important.
5.Regular Meal Timing:
Establish a consistent eating schedule with regular meal times and spacing between meals. This can help regulate blood sugar levels and support better glycemic control. Avoid skipping meals or going long periods without eating, as this can lead to imbalances in blood sugar and energy levels.
6.Monitoring and Adjusting:
Regularly monitor your blood sugar levels and assess how different foods affect your body. Keep a food diary to track your meals, portion sizes, and corresponding blood sugar readings. This will help you identify patterns, make necessary adjustments, and gain insights into what works best for your individual needs.
7.Hydration:
Stay hydrated by consuming an adequate amount of water throughout the day. Water is essential for various bodily functions and can help regulate blood sugar levels. Limit the consumption of sugary beverages and opt for water, unsweetened tea, or infused water as your main sources of hydration.
8.Seeking Professional Guidance:
It’s beneficial to consult with a healthcare professional or registered dietitian who specializes in diabetes management. They can provide personalized guidance, take into account your medical history, medications, and lifestyle factors, and help you design an eating plan that aligns with your specific needs and goals.
Remember that everyone’s dietary needs are unique, and it may take some trial and error to find the eating plan that works best for you. Be patient, stay consistent, and make gradual changes that are sustainable in the long term.
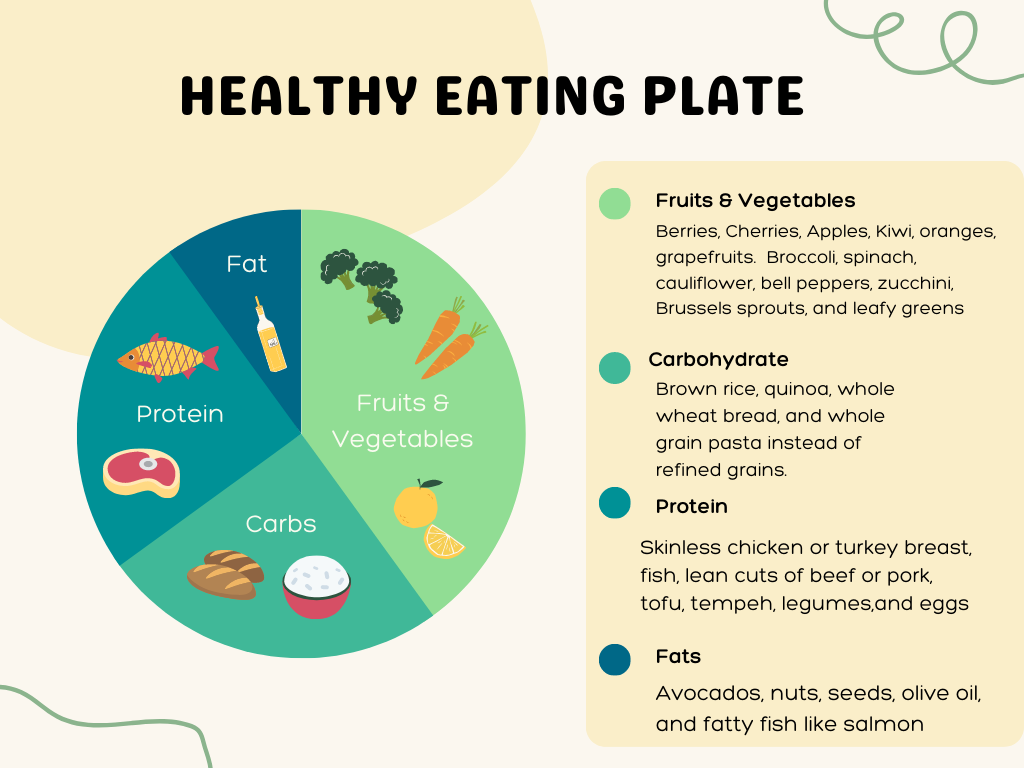
The Plate Method for Balanced Meals
The plate method is a practical and effective approach to creating balanced meals for individuals with type 2 diabetes. It provides a visual guide to help you portion your plate with the right amounts of different food groups, ensuring a well-rounded and nutritious meal.
Here’s how you can use the plate method to design balanced meals:
1.Divide Your Plate:
Mentally divide your plate into three sections: one half, one quarter, and one quarter.
2.Fill Half Your Plate with Non-Starchy Vegetables:
Non-starchy vegetables, such as leafy greens, broccoli, peppers, zucchini, and mushrooms, should occupy half of your plate. These vegetables are low in carbohydrates and calories but rich in fiber, vitamins, and minerals. They provide essential nutrients and help promote satiety without significantly impacting blood sugar levels.
3.Allocate One Quarter of Your Plate to Lean Proteins:
Choose lean sources of protein, such as skinless poultry, fish, lean cuts of beef or pork, tofu, tempeh, or legumes, and fill one quarter of your plate with these options. Proteins are vital for muscle maintenance, repair, and overall health. They contribute to feelings of fullness and help stabilize blood sugar levels.
4.Reserve the Remaining Quarter for Whole Grains or Starchy Vegetables:
The remaining quarter of your plate can be dedicated to whole grains or starchy vegetables. Choose high-fiber options like quinoa, brown rice, whole wheat bread or pasta, sweet potatoes, or corn. These choices provide energy, fiber, and important nutrients, but it’s important to be mindful of portion sizes to avoid excessive carbohydrate intake.
5.Include a Serving of Healthy Fat:
Incorporate a small serving of healthy fat, such as a tablespoon of olive oil, a handful of nuts or seeds, or half an avocado, into your meal. Healthy fats provide essential fatty acids, support satiety, and contribute to heart health. However, remember that fats are calorie-dense, so portion control is key.
6.Add a Serving of Low-Fat Dairy or Dairy Alternatives (Optional):
If you tolerate dairy products well, you can include a serving of low-fat dairy or dairy alternatives like unsweetened almond milk, Greek yogurt, or cottage cheese. These options provide calcium, protein, and other essential nutrients. Be mindful of added sugars in flavored dairy products and choose unsweetened options whenever possible.
7.Hydration and Beverage Choices:
Alongside your meal, remember to hydrate with water or unsweetened beverages. Limit the consumption of sugary drinks, fruit juices, and sweetened beverages, as they can significantly impact blood sugar levels.
The plate method offers a simple and practical way to structure your meals, ensuring a balanced intake of carbohydrates, proteins, vegetables, and healthy fats. It promotes portion control, a variety of nutrient-dense foods, and can help manage blood sugar levels effectively.
Allocating Portion Sizes for Carbohydrates, Protein, and Vegetables
When designing a healthy eating plan for managing type 2 diabetes, it’s important to allocate appropriate portion sizes for carbohydrates, protein, and vegetables.
1.Carbohydrates:
Carbohydrates have the most significant impact on blood sugar levels, so it’s crucial to manage portion sizes effectively. Aim to include controlled portions of carbohydrates in your meals. Here are some examples:-
- Starchy vegetables (e.g., potatoes, corn): Limit to about ½ cup or one small-medium-sized piece.
- Whole grains (e.g., rice, pasta, quinoa): Opt for about ½ cup cooked or one small whole grain roll.
- Bread: Choose one slice of whole grain bread.
- Legumes (e.g., beans, lentils): Limit to around ½ cup cooked.
- Fruit: Stick to one small piece or about ½ cup of chopped fruit.
- Dairy (e.g., milk, yogurt): Select low-fat options and limit to about ½ cup or one small container.
2.Protein:
Protein is essential for maintaining muscle mass and regulating blood sugar levels. Aim to include lean sources of protein in your meals. Here are some examples:-
- Poultry (e.g., chicken, turkey): Consume a portion that is approximately the size of your palm (3-4 ounces).
- Fish: Opt for a portion that is about the size of your palm (3-4 ounces).
- Lean cuts of beef or pork: Choose a portion that is about the size of your palm (3-4 ounces) and trim visible fat.
- Tofu or tempeh: Include a portion that is about the size of your palm (3-4 ounces).
- Legumes (e.g., beans, lentils): Limit to about ½ cup cooked.
- Eggs: Consume about 2-3 whole eggs or 3-4 egg whites.
3.Vegetables:
Non-starchy vegetables are low in carbohydrates and calories while being rich in fiber and essential nutrients. These should comprise a significant portion of your plate. Here are some examples:-
- Leafy greens (e.g., spinach, kale): Consume a serving that fills up most of your plate.
- Cruciferous vegetables (e.g., broccoli, cauliflower): Aim for about 1 cup cooked or raw.
- Bell peppers, zucchini, mushrooms: Include about 1 cup cooked or raw.
- Tomatoes, cucumbers, onions: Add about ½ cup or more to your plate.
By allocating appropriate portion sizes for carbohydrates, protein, and vegetables, you can create balanced meals that support blood sugar control, provide essential nutrients, and contribute to overall health and well-being.
Incorporating a Variety of Food Groups for Optimal Nutrition
Incorporating a variety of food groups is essential for achieving optimal nutrition, especially when managing type 2 diabetes. By including a wide range of nutrient-dense foods, you can ensure that your body receives a diverse array of vitamins, minerals, and macronutrients necessary for overall health and well-being.
The key is to strike a balance between carbohydrates, proteins, healthy fats, and non-starchy vegetables. Carbohydrates provide energy, and it’s important to choose complex carbs like whole grains and legumes while controlling portion sizes. Protein is vital for muscle maintenance and blood sugar control, so opt for lean sources like poultry, fish, and legumes.
Healthy fats, such as avocados and nuts, support heart health and provide satiety. Non-starchy vegetables are low in carbs and calories but high in fiber and essential nutrients. By incorporating these food groups into your meals, you can create a well-rounded and nutritious eating plan that promotes stable blood sugar levels, supports cardiovascular health, and provides all the necessary components for optimal nutrition.
Remember to consult with a healthcare professional or registered dietitian to personalize your meal plan based on your specific needs and goals.
Meal Planning Strategies for Diabetes Management: Tips for Meal Prepping and Batch Cooking
Meal prepping and batch cooking are valuable strategies that can save time, promote healthier eating habits, and support effective diabetes management. Here are some tips to help you incorporate these practices into your routine:
1.Plan your meals:
Start by creating a meal plan for the week. Consider your schedule, dietary preferences, and nutritional needs. Select recipes that incorporate a balance of carbohydrates, proteins, healthy fats, and non-starchy vegetables. Make a shopping list based on your meal plan to ensure you have all the necessary ingredients.
2.Set aside dedicated time:
Allocate a specific time each week for meal prepping and batch cooking. This could be on the weekends or a day when you have more free time. Treat it as a regular appointment and commit to it.
3.Choose diabetes-friendly recipes:
Look for recipes that are specifically designed for diabetes management. These recipes often focus on whole, unprocessed ingredients, appropriate portion sizes, and balanced macronutrient ratios. There are numerous online resources, cookbooks, and apps available that offer diabetic-friendly recipes.
4.Prepare staple ingredients:
Begin by preparing staple ingredients that can be used in multiple recipes throughout the week. For example, cook a batch of whole grains (such as quinoa or brown rice), roast a variety of vegetables, and grill or bake lean proteins like chicken or tofu. These pre-cooked ingredients can be easily incorporated into different meals.
5.Portion and store:
After cooking your meals or prepping individual ingredients, portion them into appropriate serving sizes. Use meal prep containers or storage containers that are freezer-safe and stackable. Label the containers with the name of the dish and the date it was prepared.
6.Consider freezing:
If you are prepping meals for longer periods, consider freezing them. Divide the meals into individual portions and store them in the freezer. This way, you can have ready-to-eat meals available for busy days or when you don’t feel like cooking.
7.Mix and match:
Don’t be afraid to mix and match the prepped ingredients to create different meals. For example, combine pre-cooked vegetables with cooked proteins and whole grains for a quick and balanced stir-fry. Add sauces or seasonings to enhance the flavors.
8.Utilize slow cookers or pressure cookers:
Slow cookers and pressure cookers can be incredibly helpful for batch cooking. They allow you to cook larger quantities of food with minimal effort. Consider making soups, stews, or chili in these appliances, which can be portioned and stored for multiple meals.
9.Stay organized:
Keep your prepped meals and ingredients organized in the refrigerator and freezer. Label them clearly and arrange them in a way that makes it easy to find what you need. Use transparent containers or storage bags to see the contents at a glance.
10.Enjoy the convenience:
Embrace the convenience that meal prepping and batch cooking offer. Not only do these practices save time during busy weekdays, but they also promote healthier choices by having nutritious meals readily available. You’ll be less likely to resort to unhealthy takeout or processed foods.
Creating a Schedule for Regular Eating Habits
Establishing a regular eating schedule is important for managing type 2 diabetes. Consistency in meal timing can help regulate blood sugar levels, prevent overeating, and support overall health.
Here are some tips for creating a schedule for regular eating habits:-
1.Determine the number of meals and snacks:
Decide on the number of meals and snacks that work best for you. While the standard recommendation is three meals with one or two snacks, you can adjust it based on your personal preferences and lifestyle. Some individuals may find that three larger meals without snacks work well, while others prefer smaller, more frequent meals.
2.Space out your meals and snacks:
Aim to have regular intervals between meals and snacks. This helps maintain steady blood sugar levels throughout the day. Ideally, space your meals and snacks evenly, with intervals of approximately 3 to 4 hours between each.
3.Start with a balanced breakfast:
Begin your day with a balanced breakfast within an hour or two of waking up. Including a combination of carbohydrates, proteins, and healthy fats can provide sustained energy and help control blood sugar levels throughout the morning.
4.Plan mid-morning and afternoon snacks:
If you opt for snacks, plan to have them in between meals. This can help prevent extreme hunger and overeating during your main meals. Choose snacks that are balanced, incorporating protein, fiber, and healthy fats to promote satiety and stable blood sugar levels.
5.Consistent meal times:
Establish consistent meal times that work for your daily routine. This can help regulate your body’s internal clock and enhance digestion. Try to have your meals at similar times each day, making adjustments based on your schedule as needed.
6.Allow for mindful breaks:
Allocate dedicated time for meals and snacks. Avoid eating on the go or while engaging in other activities. Instead, sit down, savor your food, and eat mindfully. This practice can help you better recognize hunger and fullness cues, leading to more balanced eating habits.
7.Include an evening meal:
Ensure that you have a well-balanced evening meal to provide nourishment and support blood sugar control throughout the night. Aim to have your last meal at least two to three hours before bedtime to allow for proper digestion.
8.Listen to your body’s hunger cues:
Pay attention to your body’s signals of hunger and fullness. Eat when you’re genuinely hungry and stop eating when you’re comfortably satisfied. This intuitive approach can help establish a healthy relationship with food and prevent unnecessary overeating.
9.Stay hydrated:
In addition to regular meals and snacks, remember to drink water throughout the day to stay hydrated. Adequate hydration supports overall health and can help regulate appetite.
10.Customize based on your needs:
Every individual is unique, and the best eating schedule may vary from person to person. Consider your personal preferences, work schedule, medication timing, and any specific dietary requirements when creating your eating schedule. Adjustments may be necessary based on your individual circumstances.
Healthy food choices for type 2 diabetes - Low Glycemic Index Foods and Their Impact on Blood Sugar
Healthy food choices for type 2 diabetes include incorporating low glycemic index (GI) foods into your diet. The glycemic index is a scale that ranks carbohydrate-containing foods based on how quickly they raise blood sugar levels. Low GI foods have a slower and more gradual impact on blood sugar, helping to keep it stable. These foods include whole grains like oats, quinoa, and brown rice; non-starchy vegetables such as broccoli, spinach, and peppers; legumes like lentils and chickpeas; and most fruits like berries, apples, and oranges.
By choosing low GI foods, you can support better blood sugar control, promote satiety, and provide a steady release of energy throughout the day. It’s important to note that portion control and overall carbohydrate intake should still be considered, even when consuming low GI foods, as they can still affect blood sugar levels. Consulting with a healthcare professional or registered dietitian can help you determine the appropriate amount and combination of low GI foods to include in your personalized healthy eating plan.
Importance of Fiber-Rich Foods for Managing Diabetes
Fiber-rich foods play a crucial role in managing type 2 diabetes and promoting overall health. Here are some key reasons why incorporating fiber into your diet is important:-
1.Blood sugar control: Fiber can help regulate blood sugar levels by slowing down the absorption of glucose. It forms a gel-like substance in the digestive tract, which slows down the release of sugars into the bloodstream. This helps prevent rapid spikes in blood sugar levels after meals, promoting more stable glycemic control.
2.Improved insulin sensitivity: High-fiber diets have been associated with improved insulin sensitivity. Insulin is the hormone responsible for regulating blood sugar levels, and increased sensitivity means the body can use insulin more effectively, leading to better blood sugar control.
3.Increased satiety and weight management: Foods rich in fiber tend to be more filling and satisfying. They add bulk to meals without adding excess calories. By promoting a feeling of fullness, fiber-rich foods can help prevent overeating and aid in weight management. Maintaining a healthy weight is important for managing type 2 diabetes.
4.Heart health benefits: A diet high in fiber has been linked to a reduced risk of heart disease, which is a common concern for individuals with diabetes. Soluble fiber, in particular, can help lower cholesterol levels by binding to cholesterol in the digestive tract and preventing its absorption into the bloodstream.
5.Digestive health: Fiber promotes a healthy digestive system by adding bulk to stools and preventing constipation. It can help regulate bowel movements and maintain regularity, which is beneficial for individuals with diabetes who may experience digestive issues.
To incorporate more fiber into your diet, focus on consuming whole, unprocessed foods such as fruits, vegetables, whole grains, legumes, nuts, and seeds. Aim for a variety of fiber sources and gradually increase your intake to allow your body to adjust. It is also important to drink plenty of water when consuming a high-fiber diet to aid in digestion.
However, it’s essential to work with a healthcare professional or registered dietitian to determine the appropriate amount of fiber for your individual needs, as too much fiber or rapid increases in intake may cause digestive discomfort or interfere with certain medications.
Building a Balanced Plate: Carbohydrate Choices for Blood Sugar Control
When it comes to managing blood sugar levels, choosing the right carbohydrates is essential. Incorporating whole grains and legumes into your diet can provide numerous benefits. Additionally, understanding the glycemic index (GI) and glycemic load (GL) can help guide your carbohydrate choices for better blood sugar control.
Whole Grains:
Whole grains are unrefined grains that contain all parts of the grain, including the bran, germ, and endosperm. They are rich in fiber, vitamins, minerals, and antioxidants. Here are some benefits of including whole grains in your diet:
- Fiber content: Whole grains are excellent sources of dietary fiber, including both soluble and insoluble fiber. This fiber helps slow down the digestion and absorption of carbohydrates, leading to a more gradual rise in blood sugar levels after meals.
- Nutrient density: Whole grains provide essential nutrients like B vitamins, magnesium, and selenium. These nutrients are important for overall health and play a role in energy metabolism and blood sugar regulation.
- Satiety and weight management: Due to their fiber content, whole grains can promote a feeling of fullness and help control appetite. This can aid in weight management, as it may prevent overeating and snacking on high-sugar foods.
Legumes:
Legumes, such as lentils, beans, and chickpeas, are nutrient-dense sources of carbohydrates that offer several benefits for blood sugar control:
- High fiber content: Legumes are rich in soluble and insoluble fiber, which slows down the digestion and absorption of carbohydrates. This helps prevent rapid spikes in blood sugar levels.
- Protein content: Legumes are also excellent sources of plant-based protein. Including protein with carbohydrates can further slow down digestion, reduce the impact on blood sugar levels, and promote satiety.
Glycemic Index and Glycemic Load:
The glycemic index (GI) is a scale that ranks carbohydrates based on their potential to raise blood sugar levels. Foods with a high GI value are digested and absorbed more quickly, leading to a rapid increase in blood sugar levels. On the other hand, foods with a low GI value are digested and absorbed more slowly, resulting in a slower rise in blood sugar levels.
The glycemic load (GL) takes into account both the quality (GI value) and quantity of carbohydrates in a food. It provides a more accurate representation of how a specific food affects blood sugar levels because it considers the serving size as well.
Remember that portion control is still important, even when consuming low GI and GL foods. Work with a healthcare professional or registered dietitian to determine the appropriate serving sizes and individualize your carbohydrate intake based on your specific needs, medications, and activity levels.
Protein Sources and Portion Control: Lean Meats, Poultry, Fish, and Vegetarian Options
Balancing protein intake with other macronutrients is crucial for a healthy eating plan, especially for individuals with type 2 diabetes. Including lean meats, poultry, fish, and vegetarian options can provide high-quality protein while keeping saturated fat intake in check. Here’s a summary of protein sources and portion control:-
1.Lean Meats and Poultry:
Choose lean cuts of meat, such as skinless chicken breast, turkey, and lean cuts of beef or pork. These protein sources are low in saturated fat and can be part of a balanced meal. Trim visible fat and remove skin before cooking to reduce saturated fat content.
2.Fish and Seafood:
Include fatty fish like salmon, mackerel, and trout, which are rich in omega-3 fatty acids, a type of healthy fat that has been linked to heart health benefits. Other fish and seafood options like cod, tuna, shrimp, and shellfish are also excellent sources of protein.
3.Vegetarian Protein Sources:
If you prefer vegetarian options or are looking to reduce meat consumption, there are plenty of plant-based protein sources available. These include legumes (beans, lentils, chickpeas), tofu, tempeh, edamame, seitan, and plant-based protein powders. Nuts, seeds, and their butters (almond butter, peanut butter) also provide protein, but they are higher in fat, so portion control is important.
Portion Control:
While protein is an essential macronutrient, it’s important to balance its intake with carbohydrates and fats. Here are some tips for portion control:
1.Be mindful of portion sizes: Aim to have a serving of protein that is about the size of your palm or deck of cards. This guideline helps ensure you’re getting an adequate amount without going overboard.
2.Distribute protein throughout the day: Include protein sources in each meal and snack to promote satiety and support muscle maintenance. This can help prevent large fluctuations in blood sugar levels and provide sustained energy.
3.Consider protein quality: Choose lean or low-fat protein sources to minimize saturated fat intake. For example, opt for skinless poultry, lean cuts of meat, and fish instead of higher-fat options.
4.Combine with other macronutrients: Pair protein with carbohydrates and healthy fats to create balanced meals. This combination can help slow down the digestion and absorption of carbohydrates, leading to more stable blood sugar levels.
Remember to individualize your protein intake based on your specific needs, dietary preferences, and any recommendations from your healthcare professional or registered dietitian. They can help you determine the appropriate amount of protein to include in your healthy eating plan while considering other aspects of your diabetes management.

Incorporating Healthy Fats
Including healthy fats in your diet is important for managing type 2 diabetes. Plant-based fats, as well as nuts, seeds, and oils, offer numerous benefits for diabetes management. Here’s a summary of incorporating healthy fats into your eating plan:-
1.Plant-Based Fats:
Plant-based fats, such as those found in avocados, olives, and coconuts, are beneficial for diabetes management. They provide monounsaturated and polyunsaturated fats, which can help improve insulin sensitivity, reduce inflammation, and support heart health. These fats are also typically low in saturated fat.
2.Nuts and Seeds:
Nuts and seeds are excellent sources of healthy fats, fiber, and important nutrients. Including almonds, walnuts, chia seeds, flaxseeds, and hemp seeds in your diet can provide omega-3 fatty acids and promote heart health. They can also contribute to feelings of fullness and help regulate blood sugar levels.
3.Healthy Oils:
Using healthy oils in cooking and dressings can add flavor and provide beneficial fats. Extra virgin olive oil, avocado oil, and coconut oil are good options. These oils contain monounsaturated and polyunsaturated fats, which have been shown to improve insulin sensitivity and support overall health. However, it’s important to use oils in moderation due to their high calorie content.
When incorporating healthy fats, it’s crucial to practice portion control and consider your overall calorie intake. Fats are more calorie-dense than carbohydrates and protein, so it’s important to strike a balance.
Here are some tips to keep in mind:-
- Measure portions: Use measuring spoons or a food scale to accurately portion out oils, nuts, and seeds. This helps control calorie intake and prevents excessive consumption.
- Choose unsaturated fats: Opt for unsaturated fats, such as those found in plant-based sources and oils, over saturated fats. Limit your intake of saturated and trans fats, as they can negatively impact heart health.
- Variety is key: Include a variety of healthy fats in your diet to obtain different nutrients and benefits. Rotate between different nuts, seeds, and oils to diversify your fat sources.
- Moderation is important: While healthy fats offer benefits, they are still calorie-dense. Be mindful of portion sizes and consider your overall energy needs when incorporating fats into your meals.
Working with a healthcare professional or registered dietitian can provide personalized guidance on incorporating healthy fats into your eating plan. They can help you determine the appropriate amount and sources of fats that align with your specific needs, preferences, and overall diabetes management goals.
Making Smart Food Choices in Different Situations: Dining Out with Type 2 Diabetes
When dining out with type 2 diabetes, it’s important to make smart food choices to maintain blood sugar control and support overall health.
Here are some tips to help you navigate restaurant menus and make healthier choices:
1.Plan ahead:
- Look up the restaurant’s menu online before going. This allows you to review the options and choose a dish that aligns with your dietary needs and preferences.
- Consider selecting restaurants that offer healthier or customizable options, such as those with salad bars, grilled or steamed dishes, or a variety of vegetable-based sides.
2.Focus on portion control:
- Many restaurants serve large portions, which can lead to overeating and spikes in blood sugar levels. Consider sharing a meal with a friend or asking for a takeout container at the beginning of the meal to portion out leftovers.
- Opt for appetizer-sized portions or choose from the lunch menu if available, as they tend to be smaller than dinner portions.
3.Mindful ordering:
- Choose grilled, baked, or steamed dishes instead of fried or breaded options.
- Opt for lean protein sources like grilled chicken, fish, or lean cuts of meat.
- Include a variety of non-starchy vegetables, such as broccoli, spinach, or asparagus, to increase fiber and nutrient content.
- Limit high-fat dressings, sauces, and condiments, or ask for them on the side to control the amount you use.
- Request modifications or substitutions to make the meal more diabetes-friendly, such as replacing French fries with a side salad or steamed vegetables.
4.Be cautious with carbohydrates:
- Pay attention to carbohydrate-rich foods like bread, pasta, rice, and desserts. Consider opting for whole grain options when available.
- Choose complex carbohydrates that are high in fiber and have a lower impact on blood sugar levels, such as quinoa, brown rice, or whole wheat bread.
- Control portion sizes of carbohydrates to help manage blood sugar levels. Fill your plate with non-starchy vegetables and protein, and keep the carbohydrate portion moderate.
5.Stay hydrated:
- Avoid sugary beverages like soda or sweetened drinks. Opt for water, unsweetened tea, or sparkling water with a squeeze of lemon or lime.
- If you choose to consume alcohol, do so in moderation and be aware of its impact on blood sugar levels. Avoid sugary mixed drinks and opt for light beer, dry wine, or spirits mixed with sugar-free mixers.
It’s essential to listen to your body’s hunger and fullness cues, and to enjoy your dining experience without feeling deprived. Making healthier choices most of the time and balancing your overall diet can help support your diabetes management goals. If you’re unsure about certain menu items or need guidance, don’t hesitate to ask your server for more information or recommendations.
Strategies for Navigating Restaurant Menus
When dining out with type 2 diabetes, navigating restaurant menus can be challenging, but with the right strategies, you can make healthier choices. Here are some tips to help you navigate restaurant menus and make more diabetes-friendly decisions:-
1.Do your research:
- Look for restaurants that offer healthier options or cater to specific dietary needs. Check online reviews or ask for recommendations from others who have similar dietary restrictions.
- Review the menu ahead of time if possible. Many restaurants now provide their menus online, allowing you to plan your choices in advance.
2.Focus on balance:
- Aim for a balanced meal that includes lean protein, non-starchy vegetables, and healthy carbohydrates. Look for options that include grilled or baked protein sources like chicken, fish, or tofu, and a variety of colorful vegetables.
- Pay attention to portion sizes and avoid oversized meals. Consider ordering from the appetizer or side dish sections to control portion sizes.
3.Be mindful of preparation methods:
- Opt for grilled, baked, steamed, or broiled dishes rather than fried or breaded options. These cooking methods typically use less added fat and are healthier choices.
- Request that your food be cooked with minimal added oils or butter. You can also ask for sauces or dressings on the side, allowing you to control the amount you use.
4.Customize your order:
- Don’t hesitate to ask for modifications to suit your dietary needs. For example, request sauces or dressings on the side, substitute high-carb sides with non-starchy vegetables or salad, or ask for whole grain options when available.
- Communicate your preferences or dietary restrictions to the server, who can provide guidance or suggestions for diabetes-friendly choices.
5.Watch out for hidden sugars:
- Be mindful of hidden sugars in sauces, dressings, marinades, and condiments. Opt for options that are labeled as sugar-free or ask for them on the side to control the amount you consume.
- Limit or avoid sugary beverages, including regular soda, sweetened teas, and fruit juices. Choose water, unsweetened tea, or sparkling water as healthier alternatives.
6.Control your carbohydrate intake:
- Be mindful of carbohydrate-rich foods like bread, rice, pasta, and desserts. Consider opting for whole grain options when available.
- Balance your carbohydrate intake by including non-starchy vegetables and lean proteins on your plate. This can help minimize the impact of carbohydrates on blood sugar levels.
7.Practice portion control:
- Many restaurants serve large portions, which can contribute to overeating. Consider sharing a meal with a dining partner or ask for a takeout container at the beginning of the meal to portion out leftovers.
- Pay attention to your body’s hunger and fullness cues, and avoid feeling pressured to finish everything on your plate.
It’s important to enjoy your dining experience while making healthier choices. By planning ahead, focusing on balance, and being mindful of preparation methods and portion sizes, you can navigate restaurant menus in a way that supports your diabetes management goals.
Portion Control Tips When Eating Out
Practicing portion control when eating out is crucial for managing type 2 diabetes. Here’s a summary of tips to help you control portion sizes and make healthier choices:-
- Share or divide your meal: –Consider sharing an entrée with a dining partner or ask for a takeout container at the beginning of the meal to portion out leftovers. This helps prevent overeating and allows you to enjoy the meal without feeling obligated to finish everything.
- Choose smaller portions:- Look for options on the menu that offer smaller portion sizes or from the appetizer or lunch menu, as they tend to be more suitable for portion control. Avoid supersized or all-you-can-eat options.
- Mind your plate:- Be aware of the size of the plate and how much food is being served. Use visual cues to create a balanced plate, such as filling half of your plate with non-starchy vegetables, one-quarter with lean protein, and one-quarter with healthy carbohydrates.
- Ask for modifications:- Don’t hesitate to request modifications to suit your portion control needs. Ask for dressings, sauces, or toppings on the side, or request smaller portions of high-carbohydrate sides.
- Listen to your body: –Pay attention to your body’s hunger and fullness cues. Eat slowly, savoring each bite, and stop eating when you feel satisfied, not overly full. Avoid the temptation to finish everything on your plate simply because it’s there.
- Be mindful of liquid calories:- Watch out for high-calorie beverages, such as sugary sodas, sweetened teas, or alcoholic drinks. Opt for water, unsweetened tea, or other calorie-free options to stay hydrated without adding unnecessary calories.
- Practice mindful eating:-Engage your senses and be fully present during your meal. Take the time to enjoy the flavors, textures, and aromas of your food. This can help you recognize when you’re satisfied and prevent mindless overeating.
Portion control is about finding the right balance and listening to your body’s cues. By implementing these tips, you can make more conscious choices when eating out and maintain better control over your portion sizes, ultimately supporting your diabetes management goals.
Healthy Snacking Options for Managing Blood Sugar Levels
Choosing the right snacks is essential for managing blood sugar levels and preventing spikes or drops in glucose.
Here are some healthy snacking options that can help you maintain stable blood sugar levels:
1.Fresh Fruits:
- Fresh fruits like berries, apples, oranges, and pears are great choices as they provide natural sugars, fiber, and important nutrients. Pair them with a protein source like nuts or yogurt for added satiety.
2.Vegetables and Hummus:
- Raw vegetables like carrots, celery, bell peppers, and cherry tomatoes are low in calories and rich in fiber. Dip them in a portion-controlled serving of hummus for a satisfying snack that provides both carbohydrates and protein.
3.Nuts and Seeds:
- Almonds, walnuts, peanuts, and seeds like chia, flaxseeds, and pumpkin seeds are excellent choices for a healthy snack. They contain healthy fats, protein, and fiber, which help slow down digestion and stabilize blood sugar levels.
4.Greek Yogurt:
- Greek yogurt is rich in protein and lower in carbohydrates compared to regular yogurt. Choose plain, unsweetened options and add fresh berries or a sprinkle of cinnamon for flavor.
5.Hard-Boiled Eggs:
- Hard-boiled eggs are a convenient and protein-rich snack. They can help keep you feeling full and satisfied while providing essential nutrients.
6.Cottage Cheese:
- Cottage cheese is high in protein and low in carbohydrates. Enjoy it on its own or pair it with fresh fruit for a balanced snack.
7.Whole Grain Crackers with Nut Butter:
- Opt for whole grain crackers made with whole wheat or seeds. Pair them with a small portion of nut butter (such as almond or peanut butter) for a combination of carbohydrates, healthy fats, and protein.
8.Snack Bars:
- Look for snack bars that are specifically designed for individuals with diabetes. Choose options that are lower in added sugars, higher in fiber, and made with whole food ingredients.
9.Veggie Sticks with Guacamole:
- Enjoy sliced cucumbers, bell peppers, or carrot sticks with a side of homemade or store-bought guacamole. Avocado provides healthy fats and fiber while adding a delicious flavor.
10.Edamame:
- Edamame, young soybeans, are a nutritious snack option. They are high in protein and fiber and can be enjoyed steamed or roasted.
Portion control is crucial when snacking. Pre-portion snacks into individual servings or use small containers to avoid overeating. It’s also important to monitor your blood sugar levels and adjust your snacks accordingly. Consulting with a healthcare professional or registered dietitian can provide personalized guidance and help you determine the best snacking options for your specific needs and diabetes management goals.
Choosing Nutrient-Dense Snacks Over Processed Alternatives
When managing type 2 diabetes, opting for nutrient-dense snacks over processed alternatives is crucial for maintaining stable blood sugar levels and supporting overall health.
1.Higher Nutritional Value:
- Nutrient-dense snacks are rich in essential vitamins, minerals, and antioxidants. They provide valuable nutrients that support your body’s functions and overall well-being.
2.Sustained Energy:
- Nutrient-dense snacks provide a steady release of energy due to their balanced combination of macronutrients (carbohydrates, proteins, and fats) and fiber. This can help prevent rapid blood sugar spikes and crashes.
3.Better Blood Sugar Control:
- Snacks with a high nutrient density can help regulate blood sugar levels more effectively than processed snacks that are often high in added sugars and refined carbohydrates. Nutrient-dense snacks provide a slower release of glucose into the bloodstream, promoting more stable blood sugar levels.
4.Improved Satiety:
- Nutrient-dense snacks tend to be more filling and satisfying due to their higher fiber, protein, and healthy fat content. They can help curb hunger and reduce the likelihood of overeating later on.
Examples of Nutrient-Dense Snacks:-
1.Raw Nuts and Seeds:
- Almonds, walnuts, chia seeds, and flaxseeds are excellent choices. They are packed with healthy fats, fiber, and protein, providing sustained energy and promoting satiety.
2.Fresh Berries:
- Berries like strawberries, blueberries, and raspberries are low in sugar and high in fiber and antioxidants. Enjoy them on their own or pair them with Greek yogurt or cottage cheese.
3.Vegetable Sticks with Guacamole or Hummus:
- Crunchy carrot sticks, cucumber slices, and bell pepper strips paired with homemade guacamole or hummus make for a nutritious and satisfying snack.
4.Greek Yogurt with Chia Seeds and Berries:
- Opt for plain, unsweetened Greek yogurt and add a sprinkle of chia seeds and fresh berries for added nutrients and flavor.
5.Hard-Boiled Eggs:
- Hard-boiled eggs are an excellent source of protein and healthy fats. They make for a convenient and satisfying snack.
6.Homemade Trail Mix:
- Create a custom trail mix using a combination of raw nuts, seeds, dried fruits (without added sugars), and a small amount of dark chocolate for a sweet treat.
7.Roasted Chickpeas:
- Roast chickpeas with a sprinkle of spices like paprika, garlic powder, or cumin for a crunchy and protein-packed snack.
8.Sliced Apple with Nut Butter:
- Enjoy apple slices paired with a tablespoon of almond butter or peanut butter for a delicious combination of carbohydrates, healthy fats, and protein.
9.Cottage Cheese with Fresh Fruit:
- Cottage cheese is a good source of protein. Top it with your favorite fresh fruit, such as sliced peaches or pineapple, for added nutrients and natural sweetness.
10.Vegetable Soup:
- Enjoy a cup of homemade vegetable soup packed with a variety of vegetables for a nutrient-rich and warming snack.
Choosing nutrient-dense snacks over processed alternatives, you can support your diabetes management goals and promote overall health. These snacks provide valuable nutrients while keeping blood sugar levels stable, helping you feel satisfied and energized throughout the day. Remember to pay attention to portion sizes and adjust your snacks based on your individual needs and blood sugar levels.
Smart Snacking Strategies to Prevent Blood Sugar Spikes
When managing type 2 diabetes, incorporating smart snacking strategies is essential to prevent blood sugar spikes and maintain stable glucose levels. Here are some tips to help you snack wisely:-
1.Pair Carbohydrates with Protein or Healthy Fats:
- When snacking on carbohydrates, such as fruits or whole grains, pair them with a source of protein or healthy fats. This combination helps slow down the absorption of glucose into the bloodstream, preventing rapid spikes in blood sugar levels. For example, enjoy an apple with a handful of almonds or whole grain crackers with a slice of turkey breast.
2.Choose Fiber-Rich Foods:
- Opt for snacks that are high in fiber as they are digested more slowly, leading to a more gradual rise in blood sugar levels. Fiber also promotes feelings of fullness and can help control appetite. Examples of fiber-rich snacks include raw vegetables with hummus, chia seed pudding, or a handful of nuts and seeds.
3.Control Portion Sizes:
- Even when choosing healthy snacks, portion control is important. Be mindful of the quantity of carbohydrates you consume, especially if they have a higher glycemic index. Use measuring cups or portion containers to ensure you’re consuming an appropriate amount to avoid blood sugar spikes.
4.Read Food Labels:
- Pay attention to food labels and choose snacks that are low in added sugars and refined carbohydrates. Look for options with minimal or no added sugars, and aim for snacks that have a good balance of macronutrients, including protein and fiber.
5.Avoid Processed and Sugary Snacks:
- Steer clear of highly processed snacks like chips, cookies, and sugary beverages. These tend to be high in refined carbohydrates and added sugars, which can lead to sharp spikes in blood sugar levels. Instead, focus on whole, minimally processed foods that provide more nutrients and have a lower impact on blood sugar.
6.Plan Ahead:
- Prepare your snacks in advance to avoid reaching for unhealthy options when hunger strikes. Pack portion-controlled snacks in small containers or snack bags, and keep them readily available in your bag or desk drawer. This way, you’re prepared with healthy choices whenever you need a snack.
7.Monitor Blood Sugar Levels:
- Regularly monitor your blood sugar levels to better understand how different snacks affect your glucose levels. This information can help you make more informed choices and adjust your snack choices accordingly.
8.Stay Hydrated:
- Drinking an adequate amount of water throughout the day is important for maintaining overall health and can help prevent excessive snacking. Sometimes, feelings of hunger can actually be a sign of thirst. Stay hydrated to avoid unnecessary snacking and support your body’s overall hydration needs.
By implementing these smart snacking strategies, you can enjoy satisfying snacks while keeping your blood sugar levels in check.
Remember, it’s always beneficial to consult with a healthcare professional or registered dietitian for personalized advice tailored to your specific dietary needs and diabetes management goals.
The Role of Physical Activity in Your Healthy Eating Plan
When managing type 2 diabetes, incorporating regular physical activity into your healthy eating plan is crucial for overall well-being and improved blood sugar control. Exercise offers numerous benefits that complement a healthy diet and contribute to better diabetes management. Here are some key roles of physical activity in your healthy eating plan:-
1.Blood Sugar Regulation:
- Physical activity helps regulate blood sugar levels by increasing the uptake of glucose by muscles, improving insulin sensitivity, and reducing insulin resistance. Regular exercise can lead to better glycemic control, helping to prevent blood sugar spikes and promoting more stable glucose levels.
2.Weight Management:
- Engaging in physical activity is an effective way to manage body weight or achieve weight loss if necessary. Maintaining a healthy weight is important for diabetes management, as excess body weight can contribute to insulin resistance and difficulties in blood sugar control.
3.Increased Insulin Sensitivity:
- Exercise enhances insulin sensitivity, allowing your body to use insulin more effectively to transport glucose into cells for energy. This can help reduce insulin resistance, a common issue in type 2 diabetes, and improve overall glucose metabolism.
4.Cardiovascular Health:
- Regular physical activity has significant cardiovascular benefits. It helps improve heart health, reduces the risk of cardiovascular diseases, and lowers blood pressure and cholesterol levels. Managing diabetes involves mitigating the risk of cardiovascular complications, making exercise a crucial component of your overall plan.
5.Improved Energy Levels:
- Engaging in physical activity can boost your energy levels and alleviate feelings of fatigue often associated with diabetes. Regular exercise increases circulation and oxygen delivery, leading to improved energy production and overall vitality.
6.Stress Reduction:
- Exercise is a natural stress reliever. It helps reduce levels of stress hormones like cortisol and stimulates the release of endorphins, promoting feelings of well-being and relaxation. Managing stress is important for diabetes management, as stress can impact blood sugar levels.
7.Muscle Strength and Bone Health:
- Physical activity, particularly resistance training, promotes muscle strength and development. Strong muscles support better glucose utilization and help maintain bone density, reducing the risk of fractures and osteoporosis.
8.Long-Term Health Benefits:
- Regular physical activity has long-term health benefits beyond diabetes management. It can help prevent or manage other chronic conditions like cardiovascular disease, certain cancers, and mental health disorders.
Incorporating physical activity into your healthy eating plan doesn’t have to be complicated. Start with moderate-intensity activities such as brisk walking, cycling, swimming, or dancing. Aim for at least 150 minutes of aerobic exercise per week, spread over several days, and include strength training exercises two or more times per week.
Benefits of Exercise for Managing Type 2 Diabetes
Regular exercise is a powerful tool for managing type 2 diabetes. It offers a wide range of benefits that positively impact blood sugar control, overall health, and quality of life.
Here are some key benefits of exercise for managing type 2 diabetes:-
1.Improved Insulin Sensitivity:
- Exercise enhances insulin sensitivity, allowing your cells to utilize insulin more effectively. This means that your body can more efficiently transport glucose from the bloodstream into the cells, reducing insulin resistance and improving blood sugar control.
2.Better Blood Sugar Control:
- Engaging in physical activity helps lower blood sugar levels by increasing glucose uptake by muscles and improving glucose metabolism. Regular exercise can lead to more stable blood sugar levels, reducing the need for medication and lowering the risk of diabetes-related complications.
3.Weight Management:
- Exercise plays a crucial role in weight management, as excess body weight is a risk factor for developing type 2 diabetes. Physical activity helps burn calories, promote weight loss, and maintain a healthy weight, which can enhance insulin sensitivity and improve blood sugar control.
4.Increased Energy Expenditure:
- Exercise increases energy expenditure, helping to create an energy deficit and support weight loss if needed. It also boosts metabolism, leading to more efficient calorie burning throughout the day.
5.Cardiovascular Health:
- Regular exercise strengthens the cardiovascular system, improving heart health and reducing the risk of cardiovascular diseases, which are common complications of diabetes. It helps lower blood pressure, reduce LDL (bad) cholesterol levels, increase HDL (good) cholesterol levels, and improve overall cardiovascular fitness.
6.Stress Reduction:
- Exercise is an excellent stress-reliever. Physical activity stimulates the release of endorphins, the body’s natural feel-good hormones, which help reduce stress, improve mood, and enhance overall mental well-being. Managing stress is crucial for diabetes management, as stress can affect blood sugar levels.
7.Increased Muscle Mass and Strength:
- Resistance training, such as weightlifting or using resistance bands, helps build muscle mass and strength. Having more muscle mass improves insulin sensitivity, as muscles are more effective at utilizing glucose for energy. It also enhances overall physical function and helps support healthy bones and joints.
8.Improved Sleep Quality:
- Regular exercise has been shown to improve sleep quality, which is essential for overall health and diabetes management. Better sleep can positively influence blood sugar control and help regulate appetite and energy levels.
9.Reduced Risk of Complications:
- Engaging in regular physical activity can lower the risk of developing diabetes-related complications, such as cardiovascular diseases, neuropathy, and kidney problems. Exercise has a positive impact on multiple body systems, supporting overall health and reducing the likelihood of complications.
10.Enhanced Overall Well-being:
- Exercise has a profound impact on overall well-being. It boosts self-confidence, improves body image, reduces feelings of anxiety and depression, and enhances overall quality of life. Incorporating regular physical activity into your routine can contribute to a more positive mindset and greater self-care.
In conclusion, exercise is a vital component of managing type 2 diabetes. Its benefits extend beyond blood sugar control and encompass overall health and well-being. By incorporating regular physical activity into your routine, you can improve insulin sensitivity, maintain a healthy weight, support cardiovascular health, reduce stress, and reduce the risk of complications associated with diabetes. Stay consistent and find activities you enjoy to make exercise a sustainable and enjoyable part of your diabetes management plan.

Improving Insulin Sensitivity and Blood Sugar Control
Insulin sensitivity refers to how effectively your cells respond to insulin, the hormone responsible for regulating blood sugar levels. In type 2 diabetes, insulin resistance occurs when cells become less responsive to insulin, leading to elevated blood sugar levels. However, several lifestyle changes can improve insulin sensitivity and enhance blood sugar control.
Here are some strategies to consider: of exercise for managing type 2 diabetes:-
1.Engage in Regular Physical Activity
- Exercise plays a significant role in improving insulin sensitivity. It helps muscles take up glucose from the bloodstream more efficiently, reducing the reliance on insulin for glucose transport. Aim for a combination of aerobic exercises (such as walking, swimming, or cycling) and resistance training (using weights or resistance bands) to maximize the benefits. Strive for at least 150 minutes of moderate-intensity aerobic activity per week, along with two or more days of strength training.
2.Maintain a Healthy Weight:
- Excess body weight, especially around the abdomen, can contribute to insulin resistance. Losing weight, if necessary, can significantly improve insulin sensitivity and blood sugar control. Focus on gradual, sustainable weight loss through a combination of healthy eating and regular physical activity. Consult with a healthcare professional or registered dietitian for personalized guidance and support.
3.Follow a Balanced, Nutrient-Dense Diet:
- Consuming a diet rich in whole, unprocessed foods can help improve insulin sensitivity. Emphasize high-fiber carbohydrates (such as whole grains, legumes, and non-starchy vegetables), lean proteins (such as poultry, fish, tofu, and legumes), and healthy fats (found in avocados, nuts, seeds, and olive oil). Avoid or limit refined carbohydrates, sugary beverages, and foods high in saturated and trans fats, as they can contribute to insulin resistance and poor blood sugar control.
4.Focus on Portion Control:
- Managing portion sizes is crucial for blood sugar control and weight management. Overeating can lead to elevated blood sugar levels, while consistently consuming appropriate portions can help stabilize glucose levels. Use portion control techniques, such as measuring cups, food scales, or visual guides like the plate method, to ensure balanced meals and snacks.
5.Incorporate Regular Meal Timing:
- Consistency in meal timing can enhance blood sugar control. Aim to eat meals and snacks at regular intervals throughout the day, spaced evenly. Avoid skipping meals or having prolonged periods without food, as this can lead to imbalances in blood sugar levels. If needed, consult with a registered dietitian to create a meal plan that aligns with your lifestyle and medication regimen.
6.Get Sufficient Sleep:
- Poor sleep or inadequate sleep can affect insulin sensitivity and glucose metabolism. Aim for 7-8 hours of quality sleep each night to support optimal insulin function and overall health. Establish a regular sleep routine, create a comfortable sleep environment, and practice relaxation techniques to promote restful sleep.
7.Manage Stress Levels:
- Chronic stress can contribute to insulin resistance and blood sugar imbalances. Implement stress-management techniques such as exercise, meditation, deep breathing, or engaging in hobbies and activities you enjoy. Seek support from healthcare professionals, therapists, or support groups to develop effective stress-management strategies.
8.Monitor Blood Sugar Levels:
- Regular monitoring of blood sugar levels helps you understand the impact of lifestyle changes on your glucose control. Use a glucose meter as directed by your healthcare provider and keep a record of your readings. This information can guide adjustments to your diet, exercise, and medication regimen to optimize blood sugar control.
These strategies are general recommendations, and individual needs may vary. It’s essential to work closely with your healthcare team, including doctors, diabetes educators, and registered dietitians, to tailor a plan that suits your specific circumstances and goals. They can provide personalized guidance, monitor your progress, and make adjustments as needed to help you improve insulin sensitivity and achieve optimal blood sugar control.
Aiding Weight Management and Overall Well-being
Weight management is a crucial aspect of managing type 2 diabetes, as excess body weight can contribute to insulin resistance and difficulties in blood sugar control. Additionally, achieving and maintaining a healthy weight offers numerous benefits for overall well-being and diabetes management.
1.Follow a Balanced and Nutrient-Dense Diet:
- Focus on consuming a variety of whole, unprocessed foods that are rich in nutrients. Include plenty of fruits, vegetables, whole grains, lean proteins, and healthy fats in your meals. These foods are generally lower in calories and higher in fiber, which can help you feel fuller for longer and support weight management.
2.Portion Control:
- Pay attention to portion sizes to avoid overeating. Use measuring cups, food scales, or visual cues (such as the plate method) to ensure appropriate portions. Be mindful of high-calorie foods and limit portion sizes accordingly.
3.Practice Mindful Eating:
- Engage in mindful eating by paying attention to your body’s hunger and fullness cues. Slow down during meals, savor the flavors, and listen to your body’s signals of satiety. This can help prevent overeating and promote a healthier relationship with food.
4.Regular Physical Activity:
- Incorporate regular exercise into your routine to aid weight management and improve overall well-being. Engage in activities you enjoy, such as walking, swimming, cycling, or dancing. Aim for a combination of aerobic exercises and strength training to burn calories, build muscle, and support a healthy metabolism.
5.Hydration:
- Stay adequately hydrated by drinking plenty of water throughout the day. Water can help promote feelings of fullness and support proper digestion. Limit sugary beverages and opt for water as your primary source of hydration.
6.Adequate Sleep:
- Prioritize getting sufficient sleep each night. Lack of sleep can disrupt hunger-regulating hormones and increase cravings for high-calorie foods. Aim for 7-8 hours of quality sleep to support healthy weight management and overall well-being.
7.Stress Management:
- Chronic stress can contribute to weight gain and hinder weight management efforts. Implement stress-management techniques such as exercise, meditation, deep breathing, or engaging in hobbies and activities that help you relax. Finding healthy ways to manage stress can positively impact weight management and overall health.
8.Support System:
- Surround yourself with a supportive network of friends, family, or support groups who can encourage and motivate you on your weight management journey. Share your goals and challenges with them, and consider seeking professional support from registered dietitians or counselors specialized in diabetes management.
Be patient with yourself and celebrate small victories along the way. It’s essential to consult with your healthcare team, including doctors and registered dietitians, who can provide personalized guidance, monitor your progress, and help you navigate challenges to achieve sustainable weight management and overall well-being.
Combining Nutrition and Exercise for Optimal Diabetes Management
Managing type 2 diabetes effectively often requires a comprehensive approach that includes both nutrition and exercise. When nutrition and exercise are combined, they can have a synergistic effect on blood sugar control, weight management, and overall well-being.
Here are some key points to consider when combining nutrition and exercise for optimal diabetes management:-
1.Coordinate Timing:
Consider the timing of your meals and exercise sessions. Eating a balanced meal or snack containing carbohydrates, protein, and healthy fats before exercise can provide the necessary energy and help prevent low blood sugar during physical activity. Also, be mindful of how your body responds to exercise and adjust your meals and insulin accordingly to avoid blood sugar fluctuations.
2.Maintain Balanced Macronutrient Intake:
Ensure your nutrition plan includes a balance of carbohydrates, protein, and healthy fats. Carbohydrates provide energy for exercise, while protein supports muscle repair and recovery. Healthy fats help maintain satiety and provide essential nutrients. Work with a registered dietitian to develop a personalized meal plan that meets your specific nutritional needs while considering your exercise routine.
3.Focus on Pre- and Post-Exercise Nutrition:
Pre-exercise meals or snacks should contain easily digestible carbohydrates to provide immediate energy. Opt for options such as fruit, whole grain toast, or yogurt. Post-exercise, consuming a combination of carbohydrates and protein can help replenish glycogen stores and support muscle recovery. Consider options like a protein shake, Greek yogurt with berries, or a small turkey sandwich on whole grain bread.
4.Hydration:
Stay hydrated before, during, and after exercise. Proper hydration supports optimal physical performance, helps regulate body temperature, and aids in nutrient absorption. Drink water throughout the day and consider consuming additional fluids during intense or prolonged exercise.
5.Monitor Blood Sugar Levels:
Regularly monitor your blood sugar levels, especially before, during, and after exercise. This will help you understand how your body responds to different types and durations of physical activity. Adjust your nutrition and/or insulin doses as needed based on your blood sugar readings to maintain optimal blood sugar control.
6.Vary Your Exercise Routine:
Incorporate a combination of aerobic exercises (such as brisk walking, jogging, cycling, or swimming) and strength training activities into your routine. Aerobic exercises help improve cardiovascular health and aid in weight management, while strength training helps build muscle mass and improve insulin sensitivity. Consider working with a qualified exercise professional to develop a personalized exercise plan tailored to your abilities and preferences.
7.Consistency and Progression:
Consistency is key when it comes to both nutrition and exercise. Strive to establish regular eating patterns and exercise routines to support stable blood sugar control and overall health. Gradually progress your exercise intensity and duration over time to continue challenging your body and reaping the benefits of physical activity.
8.Regular Monitoring and Collaboration:
Regularly consult with your healthcare team, including your doctor, registered dietitian, and exercise professional. They can provide ongoing support, monitor your progress, and make necessary adjustments to your nutrition and exercise plan based on your changing needs and goals.
Combining Nutrition and Exercise for Optimal Diabetes Management
Managing type 2 diabetes effectively often requires a comprehensive approach that includes both nutrition and exercise. When nutrition and exercise are combined, they can have a synergistic effect on blood sugar control, weight management, and overall well-being.
Here are some key points to consider when combining nutrition and exercise for optimal diabetes management:-
1.Coordinate Timing:
- Consider the timing of your meals and exercise sessions. Eating a balanced meal or snack containing carbohydrates, protein, and healthy fats before exercise can provide the necessary energy and help prevent low blood sugar during physical activity. Also, be mindful of how your body responds to exercise and adjust your meals and insulin accordingly to avoid blood sugar fluctuations.
2.Maintain Balanced Macronutrient Intake:
- Ensure your nutrition plan includes a balance of carbohydrates, protein, and healthy fats. Carbohydrates provide energy for exercise, while protein supports muscle repair and recovery. Healthy fats help maintain satiety and provide essential nutrients. Work with a registered dietitian to develop a personalized meal plan that meets your specific nutritional needs while considering your exercise routine.
3.Focus on Pre- and Post-Exercise Nutrition:
- Pre-exercise meals or snacks should contain easily digestible carbohydrates to provide immediate energy. Opt for options such as fruit, whole grain toast, or yogurt. Post-exercise, consuming a combination of carbohydrates and protein can help replenish glycogen stores and support muscle recovery. Consider options like a protein shake, Greek yogurt with berries, or a small turkey sandwich on whole grain bread.
4.Hydration:
- Stay hydrated before, during, and after exercise. Proper hydration supports optimal physical performance, helps regulate body temperature, and aids in nutrient absorption. Drink water throughout the day and consider consuming additional fluids during intense or prolonged exercise.
5.Monitor Blood Sugar Levels:
- Regularly monitor your blood sugar levels, especially before, during, and after exercise. This will help you understand how your body responds to different types and durations of physical activity. Adjust your nutrition and/or insulin doses as needed based on your blood sugar readings to maintain optimal blood sugar control.
6.Vary Your Exercise Routine:
- Incorporate a combination of aerobic exercises (such as brisk walking, jogging, cycling, or swimming) and strength training activities into your routine. Aerobic exercises help improve cardiovascular health and aid in weight management, while strength training helps build muscle mass and improve insulin sensitivity. Consider working with a qualified exercise professional to develop a personalized exercise plan tailored to your abilities and preferences.
7.Consistency and Progression:
- Consistency is key when it comes to both nutrition and exercise. Strive to establish regular eating patterns and exercise routines to support stable blood sugar control and overall health. Gradually progress your exercise intensity and duration over time to continue challenging your body and reaping the benefits of physical activity.
8.Regular Monitoring and Collaboration:
- Regularly consult with your healthcare team, including your doctor, registered dietitian, and exercise professional. They can provide ongoing support, monitor your progress, and make necessary adjustments to your nutrition and exercise plan based on your changing needs and goals.
Combining proper nutrition and regular exercise, you can achieve optimal blood sugar control, manage your weight effectively, improve insulin sensitivity, and enhance your overall well-being.
Timing Meals and Snacks Around Physical Activity
Timing your meals and snacks appropriately in relation to your physical activity can play a significant role in optimizing your energy levels, blood sugar control, and overall performance during exercise. Consider the following tips for timing your nutrition around physical activity:-
1.Pre-Exercise Nutrition:
- Consume a balanced meal or snack containing carbohydrates, protein, and healthy fats approximately 1 to 3 hours before your workout. This timeframe allows for proper digestion and ensures that you have enough energy to fuel your exercise session. Include complex carbohydrates like whole grains, lean protein sources, and a small amount of healthy fats to provide sustained energy.
2.Quick Pre-Exercise Snacks:
- If you have limited time before your workout, opt for a quick pre-exercise snack about 30 minutes to an hour before your activity. Choose easily digestible carbohydrates such as a piece of fruit, a granola bar, or a small serving of yogurt. These snacks provide a quick source of energy to fuel your muscles.
3.During Exercise Nutrition:
- For shorter workouts, water is usually sufficient to stay hydrated. However, for longer-duration or intense activities lasting more than 60 minutes, consider consuming easily digestible carbohydrates during exercise to maintain blood sugar levels and provide sustained energy. Options may include sports drinks, gels, or small portions of easily digestible foods like bananas or energy bars.
4.Post-Exercise Nutrition:
- After completing your workout, prioritize replenishing your energy stores and supporting muscle recovery. Consume a post-workout meal or snack within 30 to 60 minutes, focusing on a combination of carbohydrates and protein. This aids in restoring glycogen levels and promoting muscle repair and growth. Opt for options like a protein shake, a turkey sandwich on whole grain bread, or Greek yogurt with berries.
5.Adjusting Insulin:
- If you take insulin or other diabetes medications, it may be necessary to adjust your doses based on your exercise routine. Consult with your healthcare team to determine the appropriate insulin adjustments to prevent hypoglycemia (low blood sugar) during and after exercise.
Adjusting Carbohydrate Intake Based on Exercise Intensity
The intensity and duration of your exercise can have a significant impact on your body’s need for carbohydrates, particularly in managing blood sugar levels during physical activity. Here are some considerations for adjusting your carbohydrate intake based on exercise intensity:-
1.Low to Moderate-Intensity Exercise:
- For low to moderate-intensity exercise sessions, such as leisurely walks or light aerobic activities, your body primarily relies on stored glycogen for fuel. In this case, it may not be necessary to increase your carbohydrate intake significantly before or during exercise. Aim to consume a balanced meal or snack that includes carbohydrates, protein, and healthy fats a few hours before your workout to provide sustained energy.
2.High-Intensity or Prolonged Exercise:
- High-intensity or prolonged activities, such as intense cardio workouts, long-distance running, or vigorous cycling, may require additional carbohydrates to support energy levels and prevent a drop in blood sugar during exercise. Consider consuming easily digestible carbohydrates before and/or during the workout. Examples include sports drinks, energy gels, or small portions of easily digestible foods like bananas or energy bars.
3.Experiment and Monitor:
- Everyone’s response to exercise and carbohydrate intake can vary, so it’s important to experiment and monitor your blood sugar levels closely during and after exercise. Keep track of your carbohydrate intake, exercise duration, and blood sugar readings to identify patterns and make necessary adjustments. This will help you determine the optimal amount of carbohydrates needed to maintain stable blood sugar levels without causing spikes or drops.
4.Consult with a Healthcare Professional:
- Consulting with a registered dietitian or healthcare professional who specializes in diabetes management can provide valuable guidance in adjusting your carbohydrate intake based on your exercise routine. They can help you develop an individualized plan that takes into account your specific needs, preferences, and diabetes management goals.
Tips for Staying Motivated on Your Healthy Eating Plan
Maintaining motivation is crucial when it comes to sticking to a healthy eating plan, especially when managing type 2 diabetes.
1.Set Realistic and Achievable Goals:
- Set specific, measurable, and achievable goals related to your healthy eating plan. Break down your long-term goals into smaller, short-term goals that you can track and celebrate along the way. Having clear objectives provides a sense of direction and progress, which can boost your motivation.
2.Find Your “Why”:
- Identify your personal reasons for wanting to manage your type 2 diabetes through a healthy eating plan. Whether it’s improving your overall health, preventing complications, or enhancing your quality of life, connecting with your underlying motivations can keep you focused and determined.
3.Seek Support:
- Surround yourself with a strong support system that understands your goals and encourages your progress. This can include family members, friends, or support groups. Share your journey, seek advice, and celebrate milestones together. Consider joining diabetes support groups, both online and offline, where you can connect with others who are facing similar challenges.
4.Educate Yourself:
- Stay informed about the latest research, tips, and strategies related to managing type 2 diabetes through nutrition. Knowledge empowers you to make informed decisions, understand the impact of your choices, and adapt your eating plan accordingly. Consult reliable sources, attend educational seminars, or work with a registered dietitian to enhance your understanding.
5.Celebrate Non-Scale Victories:
- Celebrate the positive changes you experience beyond just weight loss. Notice improvements in your energy levels, blood sugar control, mood, and overall well-being. Recognize the small victories, such as making healthier food choices or maintaining consistency, as they contribute to your long-term success.
6.Plan for Challenges:
- Anticipate and plan for potential challenges that may arise along your journey. Identify potential triggers or situations that might derail your healthy eating plan and brainstorm strategies to overcome them. This could include having healthy snacks readily available, finding alternative options when dining out, or seeking professional guidance when faced with specific challenges.
7.Practice Self-Care:
- Prioritize self-care activities that promote your overall well-being. Engage in stress-reducing techniques such as meditation, yoga, or hobbies that bring you joy. Taking care of your mental and emotional health plays a vital role in maintaining motivation and staying committed to your healthy eating plan.
8.Track Your Progress:
- Keep a record of your food choices, blood sugar readings, and how you feel after meals. Tracking your progress provides valuable insights into how your eating plan is affecting your diabetes management. It can also serve as a reminder of how far you’ve come, further motivating you to stay on track.
Remember, motivation may fluctuate over time. It’s normal to face occasional setbacks or experience moments of wavering determination. During such times, revisit your “why,” seek support, and remind yourself of the benefits you’ve already achieved.
By implementing these strategies and staying committed to your healthy eating plan, you can overcome challenges and maintain long-term motivation for managing type 2 diabetes effectively.
Setting Realistic Goals and Celebrating Milestones
When it comes to managing type 2 diabetes through a healthy eating plan, setting realistic goals and celebrating milestones are essential for long-term success. Realistic goals are specific, achievable targets that align with your overall health objectives.
By breaking down larger goals into smaller, manageable steps, you create a sense of progress and accomplishment along your journey. Celebrating milestones, both big and small, provides motivation and reinforces the positive changes you’re making. Whether it’s reaching a certain weight, consistently monitoring your blood sugar levels, or successfully incorporating new, healthy food choices into your meals, take time to acknowledge and celebrate these achievements.
Recognizing your progress not only boosts your self-confidence but also reinforces your commitment to continued success. Remember, managing type 2 diabetes is a lifelong journey, and setting realistic goals and celebrating milestones help you stay motivated and focused on your long-term health and well-being.
Finding Support from Friends, Family, or Diabetes Support Groups
Navigating the challenges of managing type 2 diabetes can be easier when you have a strong support system in place. Seeking support from friends, family, or diabetes support groups can make a significant difference in your journey towards a healthy eating plan. Friends and family members who understand and support your goals can provide encouragement, accountability, and practical assistance. They can join you in making healthier food choices, help you stay motivated, and offer emotional support during difficult times.
Additionally, diabetes support groups, both online and offline, create a sense of community by connecting you with individuals who share similar experiences and challenges. These groups provide a platform to share knowledge, exchange tips, and offer emotional support. Engaging with others who are going through similar situations can provide a sense of belonging, validation, and motivation.
Whether it’s attending local support group meetings, joining online forums, or participating in social media communities, finding support from friends, family, or diabetes support groups can help you stay motivated, share experiences, and gain valuable insights for managing type 2 diabetes effectively.
Overcoming Common Challenges in Managing Type 2 Diabetes: Dealing with Cravings and Emotional Eating
Managing type 2 diabetes involves navigating various challenges, and one common obstacle is dealing with cravings and emotional eating. Here are some strategies to help overcome these challenges:-
1.Recognize Triggers:
- Become aware of the triggers that lead to cravings or emotional eating. These triggers can include stress, boredom, sadness, or certain situations. By identifying them, you can develop strategies to address them more effectively.
2.Distract Yourself:
- When cravings strike, distract yourself with a non-food-related activity. Engage in a hobby, go for a walk, practice deep breathing, or connect with a friend. Redirecting your attention can help alleviate cravings and reduce the urge to indulge in unhealthy food choices.
3.Find Healthy Substitutes:
- Instead of giving in to unhealthy cravings, find healthier alternatives. Opt for nutrient-dense snacks like fresh fruits, vegetables with hummus, or a handful of nuts. These options can satisfy your cravings while providing essential nutrients and keeping your blood sugar levels stable.
4.Practice Mindful Eating:
- Be present and mindful when eating. Pay attention to the taste, texture, and aroma of your food. Chew slowly, savor each bite, and listen to your body’s cues of hunger and fullness. Mindful eating can help you enjoy your meals more, prevent overeating, and reduce the likelihood of emotional eating.
5.Manage Stress:
- Stress can trigger cravings and emotional eating. Implement stress management techniques such as regular exercise, meditation, or deep relaxation techniques. Finding healthy outlets for stress can reduce the desire for comfort foods.
6.Seek Support:
- Reach out to a support system that understands your challenges and can provide encouragement. Friends, family, or diabetes support groups can offer emotional support, share coping strategies, and provide motivation when dealing with cravings or emotional eating.
7.Plan Ahead:
- Plan your meals and snacks in advance to avoid impulsive food choices. Include a variety of nutritious options that satisfy your taste buds while aligning with your dietary goals. Having a well-thought-out meal plan can help minimize the likelihood of succumbing to cravings or emotional eating.
8.Practice Self-Compassion:
- Be kind to yourself and understand that managing type 2 diabetes is a journey. If you occasionally give in to cravings or experience emotional eating, forgive yourself and refocus on making healthier choices moving forward. Avoid negative self-talk and practice self-compassion as you navigate these challenges.
Handling Social Situations and Peer Pressure
Handling social situations and peer pressure can be challenging when you’re managing type 2 diabetes. It’s common to encounter situations where temptations to deviate from your healthy eating plan arise, and the pressure from friends, family, or colleagues can make it difficult to stick to your dietary goals. However, with the right strategies, you can navigate these situations effectively.
First, it’s important to communicate your needs to those around you. Let your friends, family, and colleagues know about your dietary restrictions and the importance of managing your blood sugar levels. When people understand your situation, they are more likely to be supportive and accommodating.
Planning ahead is also crucial. Before attending social events or gatherings, consider the menu in advance and identify healthier options that align with your dietary goals. If necessary, bring a dish or snack that you know is diabetes-friendly to share with others. By planning ahead, you can ensure that there are suitable options available for you.
Being mindful of portion sizes is another helpful strategy. When faced with tempting food choices, prioritize nutrient-dense options such as vegetables, lean proteins, and whole grains. Be conscious of portion sizes and consider sharing dishes or opting for smaller portions to control your intake.
In situations where you encounter peer pressure or unsolicited comments about your dietary choices, it’s important to respond assertively. Politely but firmly express your commitment to your health and explain that you are making choices that align with your specific needs. Remember, it is your health, and you have the right to prioritize it.
Seeking support from others who understand the challenges of managing type 2 diabetes can also be beneficial. Join diabetes support groups, both online and offline, where you can share experiences, gain advice, and find encouragement. Being surrounded by a supportive community can provide you with the strength and resilience to navigate social situations with confidence.
Lastly, focus on non-food activities during social gatherings. Engage in conversations, participate in games, or suggest physical activities that allow you to enjoy social interactions without solely relying on food. By shifting the focus away from food, you can reduce the temptation to indulge in unhealthy options.
Handling social situations and peer pressure requires planning, communication, assertiveness, and support. By implementing these strategies, you can stay committed to your healthy eating plan and successfully manage type 2 diabetes even in challenging social environments.
Remember to prioritize your health and well-being, and don’t be afraid to advocate for yourself and make choices that align with your specific needs.
Conclusion
In this article, we have explored the importance of creating a healthy eating plan for managing type 2 diabetes. We began by understanding the basics of type 2 diabetes and the dietary guidelines recommended for its management. We delved into the impact of diet on diabetes management, focusing on carbohydrates, protein, and healthy fats. We discussed portion control, meal timing, and the importance of assessing nutritional needs. We also emphasized the benefits of personalized guidance, setting realistic goals, and the role of support systems.
Furthermore, we explored the significance of macronutrients such as carbohydrates, protein, and healthy fats in blood sugar control, satiety, and heart health. We provided strategies for designing a healthy eating plan, including the plate method for balanced meals and portion allocation. We discussed the incorporation of a variety of food groups for optimal nutrition and provided meal planning strategies, including tips for meal prepping and batch cooking.
We addressed the challenges faced in social situations and provided strategies for navigating restaurant menus, practicing portion control, and making smart food choices. We emphasized the importance of healthy snacking options, choosing nutrient-dense foods, and implementing smart snacking strategies to prevent blood sugar spikes.
Furthermore, we discussed the role of physical activity in a healthy eating plan, highlighting its benefits for managing type 2 diabetes, improving insulin sensitivity, aiding weight management, and promoting overall well-being. We emphasized the importance of timing meals and snacks around physical activity and adjusting carbohydrate intake based on exercise intensity.
Throughout the article, we acknowledged the common challenges faced in managing type 2 diabetes, such as cravings, emotional eating, and handling social situations and peer pressure. We provided strategies for overcoming these challenges and emphasized the importance of staying motivated, setting realistic goals, celebrating milestones, and finding support from friends, family, or diabetes support groups.
In conclusion, taking control of your type 2 diabetes through a healthy eating plan is within your reach. By following the guidelines and strategies discussed in this article, you can make significant strides toward better health and improved diabetes management.
Remember, it’s a journey, and every step you take toward healthier eating habits is a step in the right direction. Embrace the power of nutrition, be proactive in your approach, and never underestimate the impact of small changes. You have the ability to make positive changes and live a vibrant, fulfilling life with type 2 diabetes. Take charge of your health, and let your healthy eating plan be the foundation for your well-being